A first in
pelvic medicine
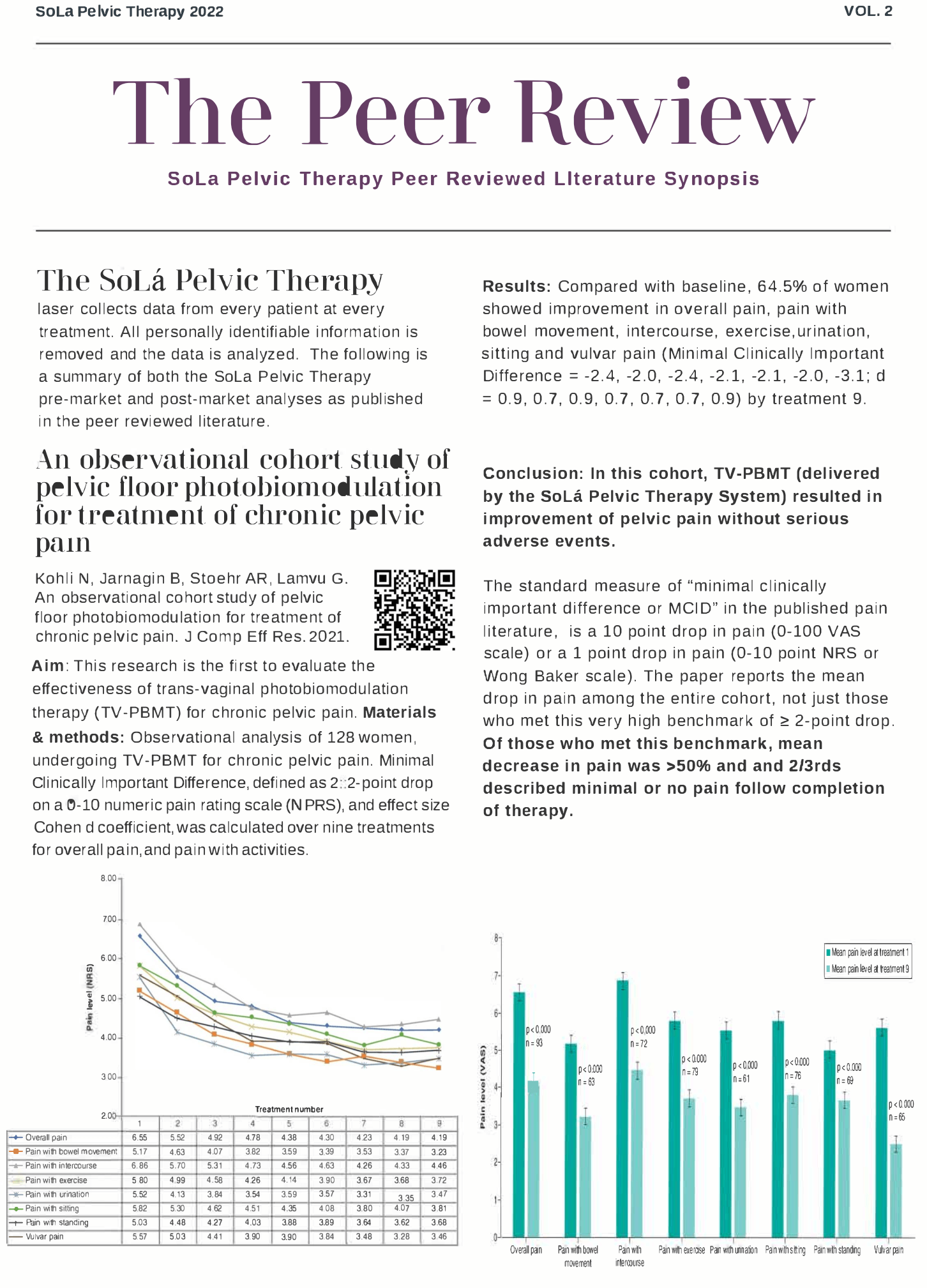
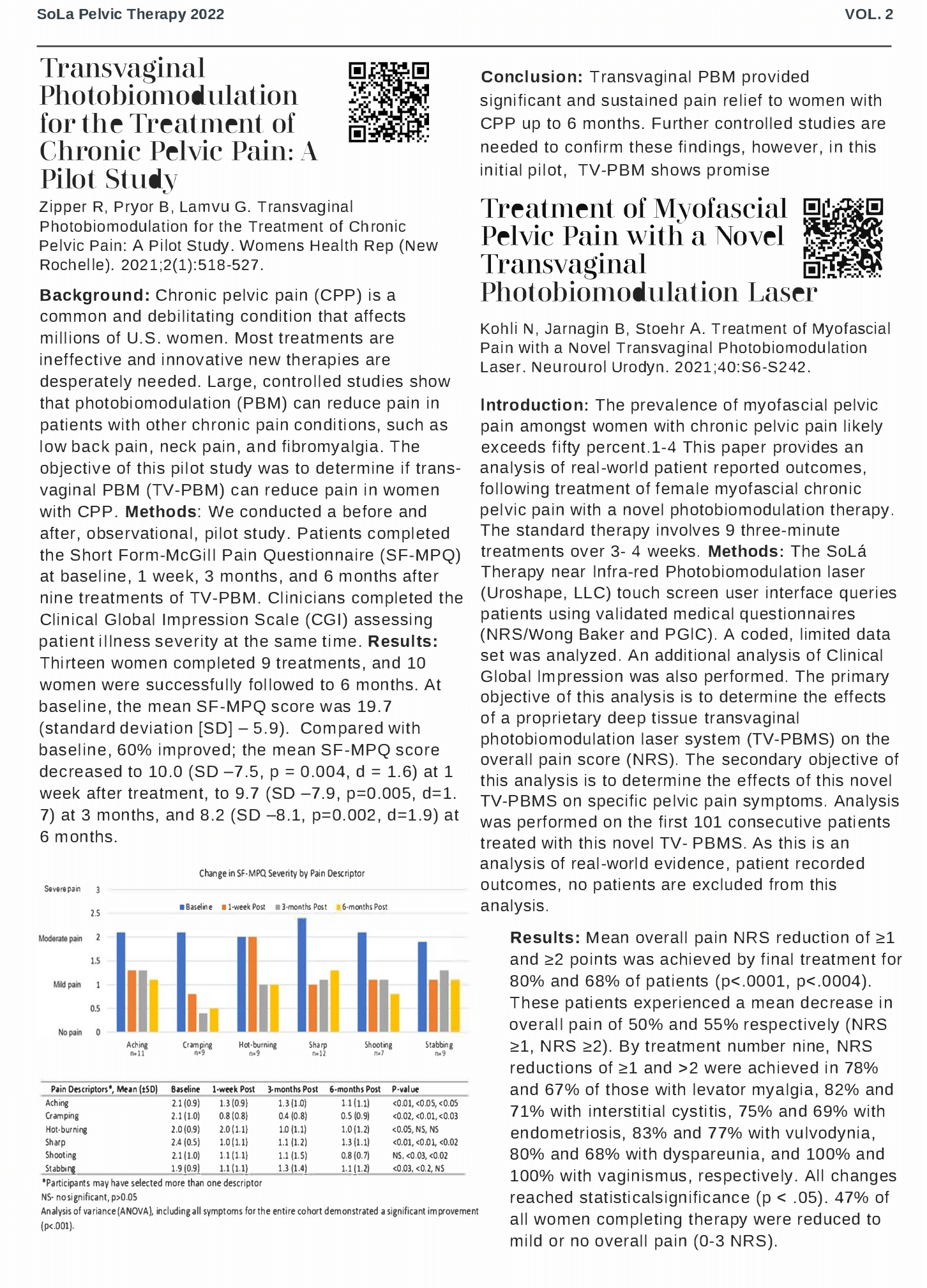
The SoLá Pelvic Therapy patient touch screen documents the responses of every patient at every treatment in every clinic. This allows patients and their health care providers to observe the changes in pain symptoms throughout the course of therapy.
Chronic Pelvic Pain and Our Data
Chronic pelvic pain conditions often overlap with nonpelvic pain disorders (eg, fibromyalgia, migraines) and non-pain comorbidities (eg, sleep, mood, cognitive impairment) to contribute to pain severity and disability. Musculoskeletal pain and dysfunction are found in 50% to 90% of patients with CPP. Although prevalence re- search is sparse, the frequency of CPP in the US is approximately 15% and it is twice as common in women as it is in men.1 In settings where women with CPP are routinely evaluated with a standardized pelvic examination, 50–90% also present with musculoskeletal pain.1-4 Myofascial pelvic pain (MFPP) and myofascial pelvic floor dysfunction are related terms used to describe musculoskeletal pelvic pain and spasm that can manifest as pain with sitting, intercourse, urination, defecation and physical activity, and is commonly associated with symptoms such as urinary urgency, frequency, constipation, sexual dysfunction or physical disability.5,6 Because of its complexity, CPP has few treatment options. Pelvic physical therapy (PT) is one of the primary treatments recommended for CPP, especially when CPP is accompanied by MFPP or myofascial pelvic floor dysfunction. However, a 2019 systematic review of PT interventions for CPP concluded that, due to heterogeneity and poor methodological quality, the evidence does not support the use of PT for the management of CPP.7
PBM uses non-ionizing light energy, in a non-thermal process, to affect the mitochondrial chromophore cytochrome c oxidase (COX). The NIR light triggers biochemical changes initiating a chain of intracellular chemical reactions.8 Nitric oxide (NO) is displaced from the mitochondria. NO is a mitochondrial waste product that is capable of binding to COX and displacing oxygen, especially in injured or hypoxic cells.9 NO is a powerful relaxer of both smooth and skeletal muscle, and it is also capable of reducing muscle pain and improving circulation to oxygen-deprived tissues.8,10,11 Additional benefits are believed to be secondary to activation of various transcription factors that result from mitochondrial stimulation as well as the modulation of reactive oxygen species.12 Unlike typical lasers that emit energy in cylindrical beams, the SoLá Pelvic Therapy Laser uses a proprietary fiber and spherical probe to emit energy as a diffuse orb.
Using HIPAA-compliant methods, our near-infrared treatment system collects data on every treatment, every day, on every patient. We collect patient-reported outcome data. This is data on every patient treated at every clinic in the U.S. We do not exclude anyone from our analyses. These analyses have been published in the peer reviewed medical literature summarized herein.
- Lamvu G, Carrillo J, Ouyang C, Rapkin A. Chronic Pelvic Pain in Women: A Review. JAMA. 2021;325(23):2381-2391.
- Fitzgerald CM, Neville CE, Mallinson T, Badillo SA, Hynes CK, Tu FF. Pelvic floor muscle examination in female chronic pelvic pain. J Reprod Med. 2011;56(3-4):117-122.
- Mieritz RM, Thorhauge K, Forman A, Mieritz HB, Hartvigsen J, Christensen HW. Musculoskeletal Dysfunctions in Patients With Chronic Pelvic Pain: A Preliminary Descriptive Survey. J Manipulative Physiol Ther. 2016;39(9):616-622.
- Sedighimehr N, Manshadi FD, Shokouhi N, Baghban AA. Pelvic musculoskeletal dysfunctions in women with and without chronic pelvic pain. J Bodyw Mov Ther. 2018;22(1):92-96.
- Bonder JH, Chi M, Rispoli L. Myofascial Pelvic Pain and Related Disorders. Phys Med Rehabil Clin N Am. 2017;28(3):501-515.
- Lamvu G, Carrillo J, Witzeman K, Alappattu M. Musculoskeletal Considerations in Female Patients with Chronic Pelvic Pain. Semin Reprod Med. 2018;36(2):107-115.
- Fuentes-Marquez P, Cabrera-Martos I, Valenza MC. Physiotherapy interventions for patients with chronic pelvic pain: A systematic review of the literature. Physiother Theory Pract. 2019;35(12):1131-1138.
- Cotler HB, Chow RT, Hamblin MR, Carroll J. The Use of Low Level Laser Therapy (LLLT) For Musculoskeletal Pain. MOJ Orthop Rheumatol. 2015;2(5).
- Brown GC. Nitric oxide regulates mitochondrial respiration and cell functions by inhibiting cytochrome oxidase. FEBS Lett. 1995;369(2-3):136-139.
- de Freitas LF, Hamblin MR. Proposed Mechanisms of Photobiomodulation or Low-Level Light Therapy. IEEE J Sel Top Quantum Electron. 2016;22(3).
- Hamblin MR. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys. 2017;4(3):337-361.
- Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516-533.
The Peer Review
Solá Pelvic Therapy Peer Reviewed Literature
Abstracts and Links To Full Manuscripts